Improving the care and outcomes for Aboriginal & Torres Strait Islander consumers with diabetes-related foot complications is the focus of a new telehealth initiative.
The project, in conjunction with the SAMHRI’s Aboriginal Chronic Disease Consortium, involves using telehealth to deliver multi-disciplinary care to patients and healthcare providers in remote and isolated areas who have active foot ulceration.
Remote communities are disproportionately affected by diabetes. Amputation rates reflect this, with much higher rates associated with Aboriginal people, rural, remote and disadvantaged communities.
The project aims to help improve outcomes for patients through awareness and early intervention. It also allows patients to remain in their communities with local supports, while receiving specialist care from a multi-disciplinary team based at the Royal Adelaide Hospital.
“Research has shown having multi-disciplinary care for this clinical presentation can reduce amputation rates by between 35-50 per cent,” Director of Podiatry, Cathy Loughry, said.
“At present patients sometimes need to travel 14 hours for an outpatient appointment, so instead we will bring the full specialist team to them with the support of their GP, local nurse or Aboriginal health practitioner.
“We can use telehealth to triage patients and monitor wounds, and where clinically appropriate we will request to see them in person.
“If we can support people to stay in their community and strengthen the skills of our Aboriginal health practitioners and other health professionals in their communities to identify issues earlier, it will result in better outcomes for patients.”
Due to the nature of foot disease, a healthcare professional needs to be present during the consult to assist with manual assessments such as dressings and or wound treatment.
The team has worked closely with the SAHMRI Aboriginal Chronic Disease Consortium and communities to ensure culturally appropriate systems are in place to maximise the use of technology to benefit patients.
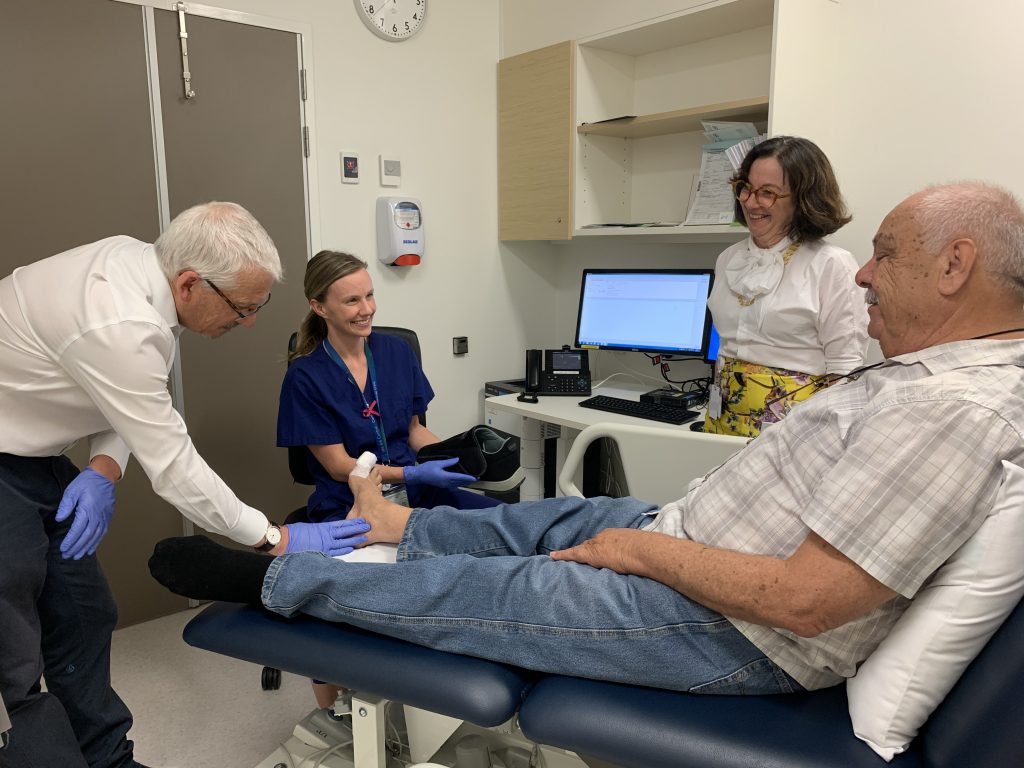
The Service aims to benefit patients like Cephas Stanley.
Cephas’s story
Port Augusta man Cephas Stanley, has made three trips to the RAH after a wound on his foot became infected.
“We’re lucky because we have accommodation with our son, but a lot of people don’t have that,” he said.
The 64-year-old who works for a not-for-profit organisation discovered he had diabetes after having a heart attack at age 34.
Managing his condition is a lifelong commitment.
“To come down here you have to take a couple of days off work, so if you don’t actually need to come here, that’s a big help,” Mr Stanley said.
“If this is utilised in Port Augusta, the APY Lands, West Coast, all the little communities, it’ll be a big help.”
Find out more about the telehealth foot service here. To access the service, a written referral is required. Referrals are accepted by all health professionals. If the matter is urgent, or if you need support completing the referral, we encourage you to phone the on-call mobile: 0479 170 999.
Pictured are Cephas Stanley with senior podiatrist Megan McAuley, Professor Rob Fitridge and Cathy Loughry.
The CALHN Aboriginal and Torres Strait Islander Diabetes-related Foot Complications Program is funded through the Indigenous Australians’ Health Programme (IAHP), a Commonwealth Government initiative.