A program to treat severe emphysema with cutting-edge technology has received a World-Class Care Award for Integrated Health Care during CALHN’s World Class Care Day.
Endobronchial valves reduce inflated lung volumes in patients with limited treatment options, and the program is one of the first of its kind in Australia.
Delivering treatment to those who need it
The pioneering technique has provided a much-needed treatment to many South Australians with chronic obstructive pulmonary disease (COPD) who would otherwise have run out of treatment options.
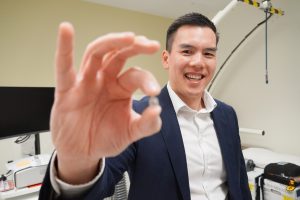
“What I like about this program is that it’s a cutting-edge program supported by a health network with good principals behind of inclusivity – so that all patients have access to this treatment,” said Professor Phan Nguyen, Head of Unit, Department of Thoracic Medicine.
“It demonstrates that this kind of complex procedure can be done in a teaching hospital and get great results.”
To date the team has treated over 50 patients at the Royal Adelaide Hospital (RAH) and reduced patient reliance on therapeutic oxygen, improved lung function, improved quality of life and functional capacity.
The program can proudly report a success rate of 80 per cent, with no deaths, greater than the best international centres who typically achieve a 70 per cent success rate.
An effective solution to a complex problem
COPD is a common condition affecting approximately 2.2 million Australians and costs the Australian community around 8.8 billion dollars per year from lost productivity, healthcare resources and welfare payments.
Emphysema is one of the conditions encompassed by COPD and involves the destruction of the air sacs responsible for gas exchange in the lungs. This damage inhibits the lungs’ ability to deflate in certain sections and results in hyperinflation, causing symptoms such as severe breathlessness, wheezing and ongoing fatigue.
Prior to the program, the standard of care for patients included vaccinations, pulmonary rehabilitation, medications, and oxygen. For patients who have completed pulmonary rehabilitation and are on maximal medical therapy (including drugs and oxygen) there are very limited options.
Surgical options such as lung transplantation or lung volume reduction exist, but carry significant risks, and many patients are medically too unwell or past the age where lung transplantation is safe.
EBVs are a relatively low-cost and safer solution, and work by blocking airflow to the most diseased parts of the lung. This allows the lung to decrease in volume and improve lung mechanics as well as a patient’s ability to breathe. The procedure can be completed within 45 mins and involves a two-day stay in hospital to monitor for complications.
The success of the program has paved the way for other public centres in Australia to build their own programs, including several hospitals in New South Wales and Victoria.
“Our program has given some momentum for other public centres to do this,” said Professor Nguyen.
The project team has also published a paper in Respiration highlighting one of their new methods of selecting the target lobe for endobronchial valve lung volume reduction.
Strength in numbers
According to Professor Nguyen, the success of the program is partly down to a close collaboration between thoracic medicine medical staff, nuclear medicine, radiology and nursing.
“It’s the teamwork that I’m most proud of,” said Professor Nguyen.
“Collaboration between our medical team, radiology, nuclear medicine, referrals from all centres, not just public or private hospitals, and our nursing team are a well-oiled machine – they could probably do it without me!”