Implementing world-best practice for spinal cord injury, and a project improving outcomes for Aboriginal patients on dialysis, are among the initiatives to receive CALHN CEO Clinical Rapid Implementation Project Scheme (CRIPS) grants.
This year four projects will each receive $200,000 to support the innovative hospital-based projects that identify real solutions and improve health service delivery.
“Research underpins everything we do, and sets us up to help meet our ambition of being in the top 5 hospitals in Australia, and within the top 50 worldwide by 2025,” CEO Lesley Dwyer said.
“Recognising the immense talent within our network, late last year I announced the CALHN CEO CRIPS and I am so impressed with large amount of high-quality expressions of interest we received through this process.
“It again shows that we have the right people here within our network to help us deliver our vision of world-class research and world-class patient care.”
The successful projects are:
- Advanced Recovery Room Care – an iterative model to improve outcomes and reduce cost in perioperative care: Professor Guy Ludbrook, Professor of Anaesthesia.
- Code Spine – the development and implementation of the world’s best for acute management of spinal cord injury: Professor Brian Freeman, Head of Spinal Services.
- Aboriginal dialysis models of care – improving health outcomes in Aboriginal patients by improving adherence to dialysis treatment: Brian Farmer, Nurse Consultant – Renal Complex Care.
- Rapid Access for atrial fibrillation – the impact of an emergency department protocol and rapid access AF clinic to reduce hospitalisations for atrial fibrillation: Professor Prashanthan Sanders, Director of Pacing and Electrophysiology.
Code Spine
There are about 253 cases of traumatic Spinal Cord Injury (SCI) in Australia each year. Prof Freeman and his team are furthering research and implementing world best emergency process to care for SCI patients, known as “Code Spine”. The model fast-tracks potential SCI patients from incident to surgery within eight hours, to help improve outcomes.
“Traumatic spinal cord injury is a life changing neurological condition with substantial socioeconomic implications for patients and their caregivers,” Prof Freeman said.
“This quality improvement initiative will require rapid assessment by paramedics, emergency consultants, radiologic investigations, operating theatre, anaesthetists, spinal surgeons, intensive care, and early rehabilitation.”
Reduce Atrial Fibrillation (AF)
AF is now the most common cause for cardiovascular hospitalisation in Australia, outnumbering those for both heart failure and heart attack.
Professor Sanders says few studies have explored strategies to reduce this.
His project will examine a unique model of care – ED protocol and a rapid access AF clinic – for the emergency management of AF.
“This intervention is expected to result in marked reductions in unnecessary hospitalisations and improved outcomes in this high-risk population,” Prof Sanders said.
Aboriginal dialysis models of care
Providing dialysis care in a culturally appropriate setting, and delivered by a workforce that is culturally and clinically capable, will improve treatment adherence and ultimately health outcomes for Aboriginal dialysis consumers.
Mr Farmer’s project involves recruitment and training of two Aboriginal Health Practitioners (AHP) in haemodialysis and supports the implementation of a two-chair dialysis service at Kanggawodli Hostel, that has been co designed using Aboriginal consumers and partners.
Advanced Recovery Room Care
Moderate-risk surgical patients at Royal Adelaide Hospital have a high incidence of early serious postoperative complications.
This affects patient wellbeing, is costly and produces a high rate of unplanned postoperative hospital re-admissions. A trial of a new model of enhanced care after surgery demonstrated that complications were quickly identified and expertly addressed, decreasing readmission days and improving patient outcomes.
Prof Ludbrook’s project builds on a previous trial and to confirm the benefits of an Advanced Recovery Room Care for orthopaedic, colorectal, gynae-oncology and neurosurgery patients.
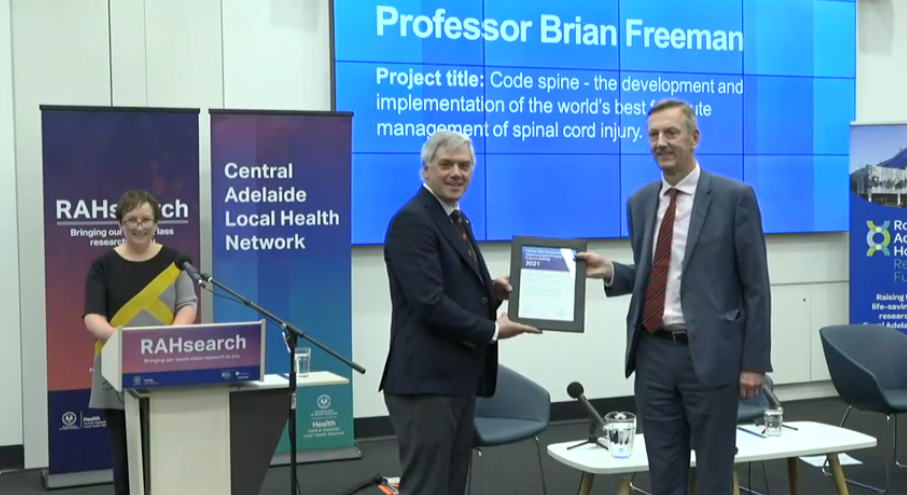
Pictured are CEO Lesley Dwyer, Head of Research Prof John Beltrame and CRIPS recipient Prof Brian Freeman.